The Case Against Specialization
On medical zebras and the nature of chronic disease
In honor of Rare Disease Day on February 28th, I thought I'd share part of my personal health journey and what I learned about chronic diseases along the way. After many months of long COVID complications that affected my heart, lungs, and kidneys, my nutritionist proposed a possible explanation for the recent resurgence of certain GI symptoms: namely persistent abdominal pain and burning, severe weight loss, and nausea.
In November 2020, I was diagnosed with superior mesenteric artery syndrome (SMAS), also known as Wilkie’s syndrome, an obstructive GI condition in which the small mesenteric artery compresses the duodenum, the first part of the small intestine, causing early satiety, nausea, vomiting, and weight loss.
The only problem was this diagnosis didn't line up with my history or presentation, but my doubts and concerns were continually swept under the rug. While structural imaging studies did reveal findings strongly suggestive of Wilkie’s syndrome, gastric emptying tests returned normal, suggesting that a GI blockage was neither present nor responsible for my alarm symptoms.
Inflammatory bowel disease (IBD) appeared a far more likely culprit based on my presentation and elevated inflammatory markers, but cognitive fallacies like diagnosis momentum and confirmation bias proved too powerful to fight.
Despite the growing mountain of evidence to the contrary, my physicians stuck to their original diagnosis, and I was scheduled to undergo an invasive operation to address the purported intestinal blockage.
Post-surgery, I dealt with many complications, including abdominal adhesions, scars that—ironically enough—really do obstruct the GI tract. The inflammation worsened, the incision site was frequently infected, and I remained dangerously emaciated.
To recover, I independently implemented dietary modifications and pursued microbiome modulation therapies such as fecal microbiota transplantation (FMT), which involves inoculating a sick person with healthy gut microbes in order to promote immune tolerance, protect against pathogen invasion, and tamp down inflammation.
Re-Defining Disease
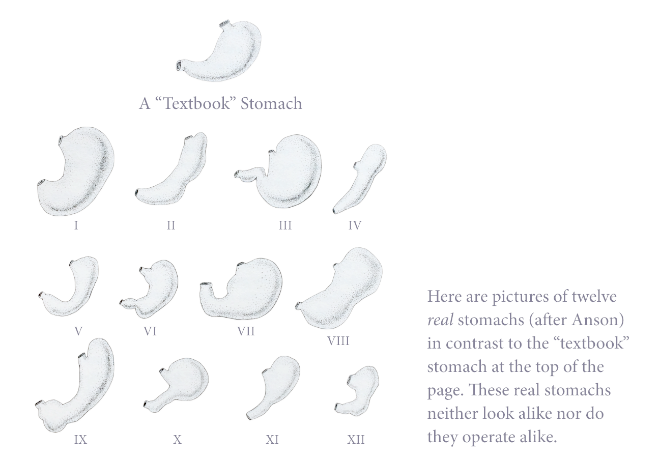
What are the main takeaways? Patients with rare diseases, or medical zebras, do exist, but accurate identification is nuanced. Sometimes, conditions that are considered detrimental are simply reflections of the normal variation observed across human populations. Medicalization of normal variation does more harm than good.
In my case, the structural abnormality of an extremely narrow aortomesenteric angle of 7° (25° to 60° is considered normal) wasn’t indicative of pathology since my transit studies were unremarkable. Most chronic diseases are functional, rather than structural, in nature. Our current system of medical specialization, based on anatomy instead of energy metabolism, often prevents effective root-cause analysis.
Body Language
A specialist focuses on an organ whose functions are studied in detail, but the communication between different systems is seldom addressed. Disease frequently arises outside of the organ presenting with symptoms, but tunnel vision can blind us to the bigger picture. “No man is an island," but neither is any organ, tissue, or cell.
Everything is interconnected as evidenced by crosstalk between organ systems. In the same way that a mechanic cannot fix a car without knowing how its parts interact, neither can a physician effectively treat disease without considering the larger ecological landscape.
Elucidating the importance of effective communication along the gut-brain axis, neurodegenerative diseases such as Alzheimer’s and Parkinson’s are associated with specific dysbiotic gut microbiota signatures. But how frequently does a neurologist consult with a gastroenterologist?
A Path Forward
How should one approach chronic complex medical cases then? Even if the exact phrase doesn't appear in the original Hippocratic Oath, our first priority should still be to do no harm. To borrow from Seneca, “Nothing is more harmful than premature treatment.”
Since energy is required to maintain and repair structures, chronic disease necessarily involves defects in energy metabolism. When multiple organ systems are involved, investigate gut microbiome dysbiosis and mitochondrial dysfunction, factors that underlie nearly all chronic disease conditions.
Gaining an appreciation for the complex biochemical pathways and symbiotic microbial ties that govern our physiology will set us on the path toward healthy longevity!




This was another important piece from you, Nita. Tomorrow, I'm scheduled for a treadmill stress echocardiogram, due to Covid damage to the lining of my blood vessels. Although my EKG appears nearly normal (nonspecific ST abnormality), and my only symptom is some chest discomfort with moderate exercise, I'm curious to see what is revealed. My treatment plan will be discussed. Doctors often "stovepipe" a patient's symptoms, not seeking other physicians' input. And Confirmation Bias is real.
I was happy to see you suing the word "recovery" here! Does this mean you're on the road back, or at least that there's light at the end of the tunnel?