A Dietary Guide to Cancer Defense
From menus and meal plans to cellular microenvironments
While cancer encompasses a wide spectrum of diseases, certain hallmarks are common among them, such as resistance to cell death, sustained proliferative signaling, and reprogramming of energy metabolism. One critical trait is acquired resistance to apoptosis.
Cancer at the Cellular Level: Apoptosis vs. Necrosis
Under normal conditions, cells that fail to pass certain checkpoints during the cell cycle are marked for programmed cell death via apoptosis, a form of cellular suicide that removes damaged or unwanted cells without causing inflammation.
Cells that die in this manner slowly shrink and leave surrounding tissue intact—“not with a bang but a whimper.” Apoptosis serves as a natural barrier to cancer development, and its suppression can promote tumor growth.
In contrast, necrosis involves the rupture of the cell membrane, leading to the release of proinflammatory cytokines into the surrounding tissue microenvironment, akin to a supernova explosion.
This process triggers inflammation and recruits immune cells to the site of damage, which stimulates angiogenesis, the formation of new blood vessels that supply oxygen and nutrients to tumors and facilitate their growth.
The tumor microenvironment consists of surrounding noncancerous cells and molecules, which are often cajoled by cancer into acting as accomplices. If a given microenvironment was characterized by apoptosis as the dominant form of cell death over necrosis, that microenvironment could preclude the development of cancer.
Key Questions
If cancer development is driven by the tumor microenvironment, how can an individual’s broader macroenvironment impact cellular microenvironments?
Can dietary choices help maintain appropriate levels of apoptosis and thus reduce cancer risk?
Cancer Is Not Caused by Mutations
“We find ourselves at the present time in the era of molecular biology, and we are perhaps unduly influenced by the genetic code as the dominant principle in biology. Perhaps, in a decade or two from now, the dominant principle may shift to another plane, which in turn will influence our speculations about tumor causation.”
The Impact of Cruciferous Vegetables on Cancer Risk
Cruciferous vegetables—such as broccoli, cabbage, kale, and Brussels sprouts—are rich in compounds that have been shown to induce apoptosis in various in breast, brain, blood, bone, colon, gastric, liver, lung, oral, ovarian, pancreatic, prostate, and skin cancer lines.
One such compound called sulforaphane, particularly abundant in broccoli sprouts, bok choy, and cabbage, also induces apoptosis in acute lymphoblastic leukemia (ALL), the most common blood cancer in children.
Optimizing Sulforaphane Intake
A 2008 randomized controlled trial found that consumption of raw broccoli resulted in faster absorption, higher bioavailability, and higher peak plasma amounts of sulforaphane compared to cooked broccoli.
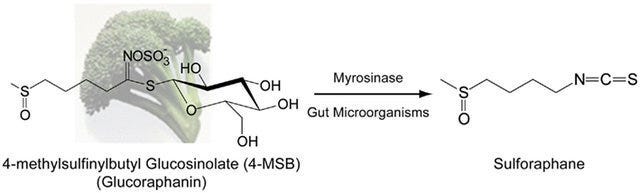
Boiling, steaming, or microwaving at high power (850–900 watts) can inactivate myrosinase—a plant enzyme essential for converting glucosinolates (like glucoraphanin) into biologically active isothiocyanates (like sulforaphane).
To enhance sulforaphane bioavailability when consuming cooked vegetables, one can:
Add powdered brown mustard seeds, a rich source of myrosinase, to cooked broccoli
Rely on colonic gut microbiota, which possess myrosinase enzymes, to facilitate the conversion of glucoraphanin to sulforaphane, albeit to a lesser extent than would occur in the small intestine
Recent studies continue to support the potential anticancer effects of sulforaphane. For example, a 2023 Frontiers in Oncology review highlighted sulforaphane's antioxidant, anti-inflammatory, cardioprotective, immunostimulant, and anti-cancer properties. However, most clinical studies are limited and focus on biomarkers rather than long-term cancer outcomes. More extensive human clinical trials are needed to fully understand the impact of sulforaphane on cancer prevention.
Resistant Starch & Colorectal Cancer Prevention
Colon cancer is the third most common type of cancer globally and remains a leading cause of cancer-related deaths. Particularly concerning is the recent rise of colon cancer among young adults. Dietary patterns significantly influence colorectal cancer risk, with fiber intake being inversely associated with disease incidence. In fact, immigrants experience an increased risk of colon cancer after moving to developed countries and converting to a Western diet.
Resistant starch (RS) refers to starch that escapes digestion in the small intestine and reaches the colon undigested, where it is fermented by gut microbiota to produce short-chain fatty acids (SCFAs) like butyrate. Butyrate serves as the primary energy source for colonic epithelial cells and has anti-inflammatory and anticancer properties. The short-chain fatty acid promotes apoptosis in mutated cells, inhibits cell proliferation, and improves gut barrier function.

Not All Fiber Is Created Equal
In contrast to other types of fiber such as non-starch polysaccharides (NSP), resistant starch may confer unique benefits and can be characterized into five types, the first three of which occur in a normal human diet:
RS1 describes starch that is physically trapped within plant cell walls and protein matrices and includes whole grains, seeds, and legumes
RS2 consists of native, granular starch and includes green bananas, raw potatoes, and high amylose corn starch
RS3 comprises retrograded starches that are formed when starchy foods (e.g. rice, potatoes, pasta, bread, cornflakes) are cooked and cooled
RS4 is composed of chemically modified starches used in the food industry to commercially produce baked goods
RS5 refers to amylose-lipid complexes, consisting of starch and fatty acids, that form during food processing, which may include the use of emulsifiers
RS2, such as raw potato starch, ferments quickly in the proximal part of the colon, and doesn’t change stool pH. On the other hand, RS3 ferments slowly all the way to the distal end of the colon and feeds SCFA-producing bacteria, thereby lowering colonic pH, preventing pathogen invasion, maintaining epithelial tissue health, and inhibiting carcinogenesis. Most of the fiber content in a typical Western diet primarily ferments in the proximal portion of the colon.
Studies have shown that individuals with colorectal cancer often possess lower levels of butyrate-producing bacteria, such as Faecalibacterium prausnitzii and Roseburia species, compared to healthy individuals. A study examining the effects of resistant starch using human gut microbiota cultures found that RS3 doubled the proportion of Bifidobacterium in the distal colon and induced higher levels of butyrate production.
The most common example of RS3 is cooked and cooled rice and potatoes, but green plantains, cassava, and taro also contain mixtures of several types of resistant starch, including RS3. Although specific daily intake recommendations for resistant starch have not been formally established, evidence suggests that:
Approximately 20 grams of resistant starch per day may confer digestive health benefits
6 to 12 grams per meal can inhibit postprandial increases in blood glucose and insulin levels
In contrast, the average American intake is estimated to be around 4.9 grams per day, slightly below the range needed to observe beneficial effects at a single meal and considerably short of the daily intake associated with health benefits.

Red Meat Consumption & Colorectal Cancer Risk
The relationship between red meat consumption and colorectal cancer has been extensively studied, with mixed findings:
Epidemiological Studies: While some studies have identified correlations between high red meat intake and increased colorectal cancer risk, a comprehensive meta-analysis of 35 prospective studies found the associations weak in magnitude and not statistically significant.
Geographical Variations: Positive associations between red meat and colorectal cancer are more frequently observed in U.S. populations compared to European and Asian cohorts. This disparity may be attributed to differences in dietary patterns, such as the consumption of red meat with refined grains, sugar-sweetened beverages, and processed oils prevalent in Western diets.
Confounding Factors: Observational studies often suffer from “healthy user bias,” where individuals who consume more red meat may also engage in other behaviors that affect cancer risk, such as smoking, alcohol consumption, and lower physical activity. These confounding factors complicate the ability to isolate the effects of red meat on cancer risk.
Potential Protective Role of Resistant Starch
Even if red meat were conclusively linked to increased colorectal cancer risk, integrating resistant starch into the diet might mitigate potential adverse effects. Resistant starch can shift colonic fermentation from protein substrates to carbohydrate substrates, enhancing SCFA production and reducing the formation of pro-inflammatory protein-derived metabolites. This shift may protect against DNA damage and carcinogenesis.
Organic Foods & Cancer Risk
The consumption of organic foods has been proposed to reduce cancer risk by minimizing exposure to pesticide residues:
Pesticides and Carcinogenesis: The International Agency for Research on Cancer (IARC) has classified certain organophosphate pesticides (e.g., glyphosate, malathion, diazinon) as probable human carcinogens (group 2A) based on studies involving occupational exposure and laboratory animals.
Observational Studies: A 2018 study published in JAMA Internal Medicine followed nearly 69,000 French adults over four years and found that individuals who primarily consumed organic foods had a 73% lower risk of developing non-Hodgkin lymphoma and a 21% lower risk of postmenopausal breast cancer compared to those who rarely ate organic foods. These findings were attributed to reduced exposure to pesticide residues.
Cautions and Considerations
Study Limitations: The study relied on self-reported dietary intake, which can introduce reporting biases, and did not fully account for confounding health behaviors, as individuals who consume organic foods might also engage in other healthy behaviors that independently reduce cancer risk.
Current Evidence: While some studies suggest a protective effect of organic foods against certain cancers, more rigorous research is needed to establish causality and control for confounding factors.
Putting It All Together
Diet may play a vital role in cancer prevention and progression. Incorporating cruciferous vegetables into the diet may provide compounds like sulforaphane that promote apoptosis and inhibit cancer cell growth. Increasing intake of resistant starch can enhance butyrate production in the colon, supporting gut health and potentially reducing colorectal cancer risk.
While the relationship between red meat consumption and colorectal cancer can’t be conclusively established, incorporating resistant starch may mitigate some adverse effects. Nonetheless, limiting red and processed meat intake is recommended.
Choosing organic foods may reduce exposure to certain pesticides, but definitive evidence linking organic food consumption to lower cancer risk is lacking. Emphasizing a diversified diet rich in plant-based foods, whether organic or conventionally grown, is critical to reducing cancer risk.
Key Takeaways
Increase consumption of cruciferous vegetables: Include raw or lightly cooked broccoli, cauliflower, Brussels sprouts, and other cruciferous vegetables to maximize sulforaphane intake.
Boost resistant starch intake: Incorporate foods high in RS, such as legumes, whole grains, cooked-and-cooled rice and potatoes, green bananas, and oats.
Limit processed meats: Ensure consumption of red meat is accompanied by adequate dietary fiber intake and avoid processed meats such as sausages.
Focus on overall dietary patterns: Adopt a balanced diet rich in fruits, vegetables, whole grains, and low in processed foods and added sugars.
Consider food preparation methods: Avoid cooking methods that may inactivate beneficial compounds or create harmful substances.
Informed dietary choices can positively influence cellular microenvironments and gut ecology in a manner that reduces the risk of different types of cancers.
Disclaimer: The information in this article is for educational purposes only and should not be considered medical advice. While diet may play a role in cancer prevention, no dietary changes can guarantee protection against cancer. Always consult qualified healthcare providers about your personal cancer risk and any dietary modifications, especially if you have existing health conditions or are undergoing treatment.



